At Withings we have a healthy respect for privacy.
Read our privacy policy
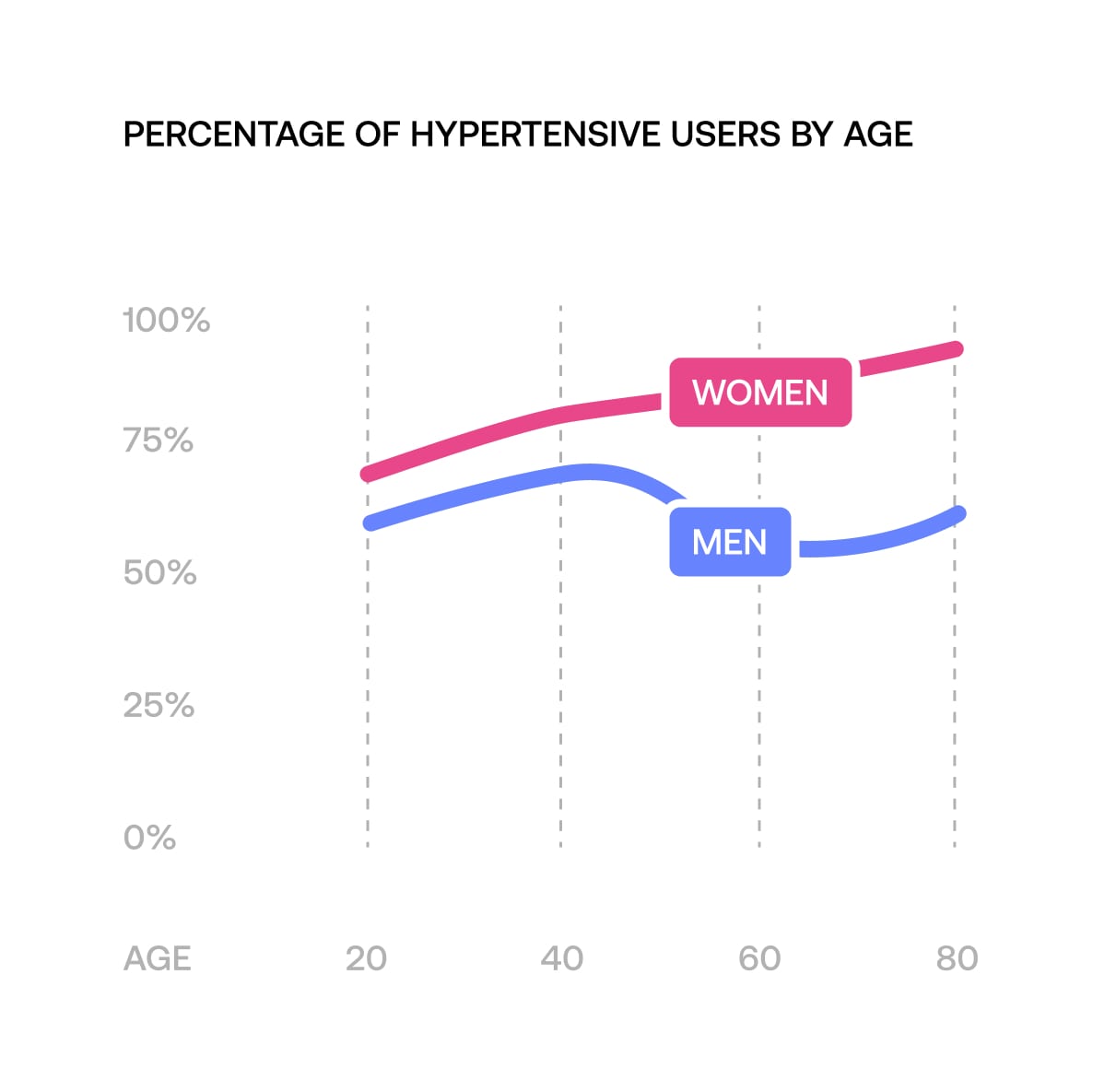
"Hypertension is the leading cause of cardiovascular diseases⁴ (such as stroke, myocardial infarction, heart failure, and fibrillation) and therefore the leading cause of death."